DURYEA, Pa. -- We featured a young woman from Luzerne County on Tuesday who says doctors saved her life using a bedside life support system called ECMO.
We got a demonstration about how it works and why doctors are using it more often.
Amanda McAndrew, 30, from Duryea, has had asthma for about half of her life.
"Maybe three years ago it started getting worse, don't know why."
She and her husband Michael shared with us earlier this week the story of how in March, she had an asthma attack so severe she passed out in the driver's seat of her car.
Doctors say a machine called ECMO saved her life.
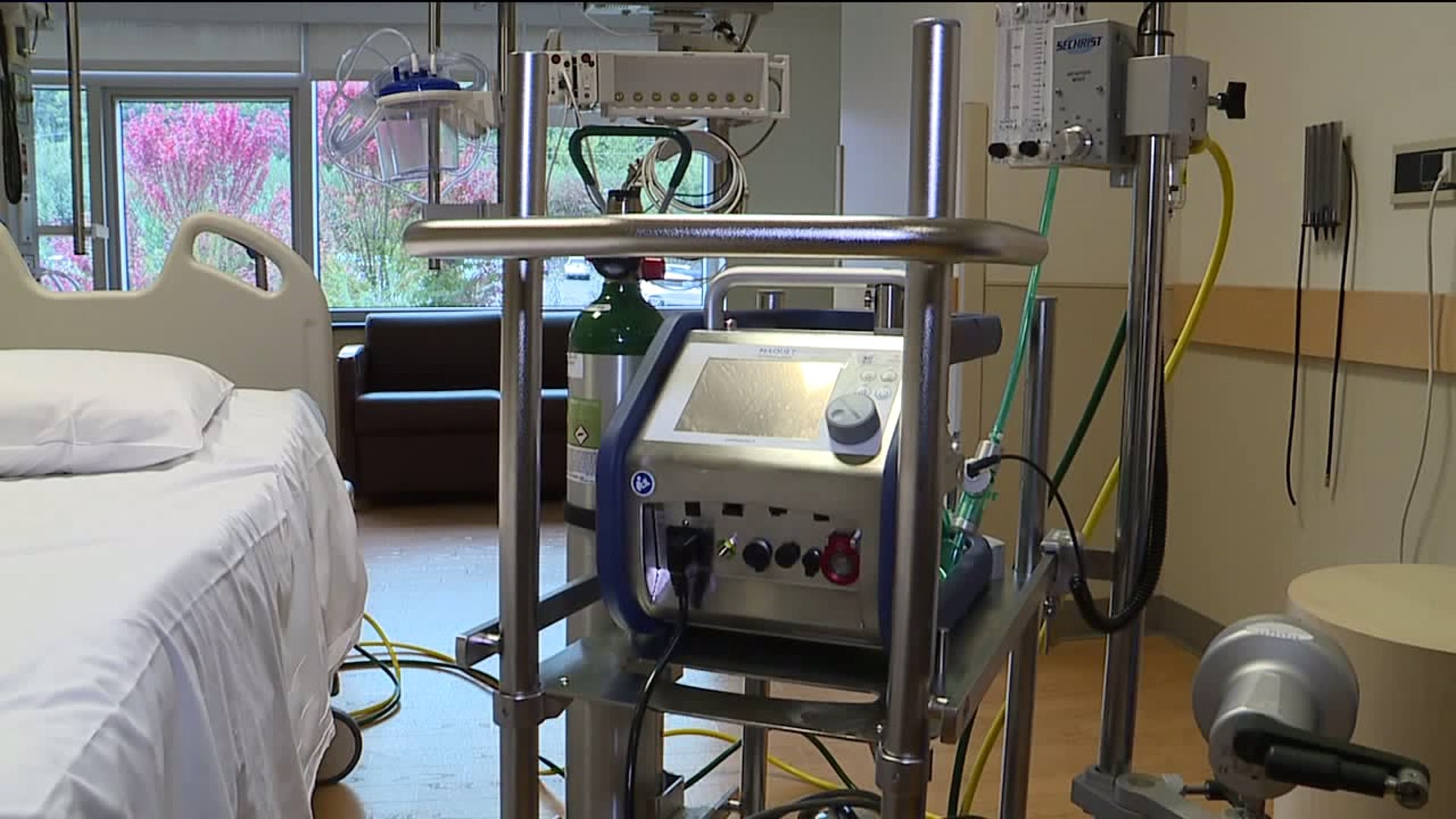
"ECMO very simply stands for extracorporeal membrane oxygenation, a fancy way of saying we take the blood out of a patient's body, put it in a machine that puts oxygen in it, and puts it back in the patient's body," explained Dr. Deepak Singh.
Dr. Singh is director of cardiothoracic surgery for Geisinger Northeast. He explains ECMO gives a patient's lungs and heart a rest, used in situations such as a drowning or a massive heart attack.
"I would say our threshold to use it has become lower," said Dr. Singh.
Evan Gajkowski is the ECMO coordinator, leading a multi-disciplinary team whose job it is to watch out for the risks such as clotting or hemorrhaging.
"If the patient is starting to improve, they'll show us that they can come off ECMO," Gajkowski said.
He showed us how it's done: after he's sure there's no air in the port, it's inserted into a patient's neck. One tube takes blood out, and after it's circulated through the machine, the other puts it back in. It can circulate anywhere from 1/3 to 2/3 of a patient's blood volume.
ECMO is technology that's been around for more than 70 years, but doctors took a second look during 2009, the year of the H1N1 flu virus. Nationwide, far more patients survived than expected, and a closer look at the numbers showed ECMO may have had something to do with that.
"You can have a very bad flu episode or superimposed with pneumonia, and your lungs could stop working," Dr. Singh said.
The patient does not need to be sedated and the average length of time on it is seven days.
Critical care physician Dr. Mary Jane Reed noted for as critical as she was, Amanda needed only a few days.
"Her heart stopped several times. They were able to restart it and keep it going until Dr. Singh was able to get ECMO in and get her on a circuit," said Dr. Reed. "After just a couple of minutes, her blood pH came almost back to normal and she became more stable."
Amanda is set to be part of an inaugural support group Geisinger is setting up for patients who have needed ECMO.
Doctors say they would love to not have new people join those ranks and stress that getting a flu shot, keeping your lungs healthy on their own, is the best thing to do right now.